Six months ago, the idea of being able to get a repeat script, a referral to a specialist and even a diagnosis from your GP from the comfort of your own couch seemed like a Silicon Valley concept we might see several years from now. But just a few months into the COVID era and many GPs think this new, convenient reality is here to stay – despite there being a common belief among GPs that it has a negative impact on managing patient care.
There are many reasons to embrace the emergence of telehealth: the social distancing benefits are undeniable when the nation is at the height of a pandemic and all human contact should be limited. And for patients without transport or challenging work schedules, having access to essential GP services without having to visit a medical centre in person is a significant convenience.
Many patients are happy with the new-found availability of services that would have once required face-to-face contact. After all, it’s one less human interaction in a world where real human interactions are disappearing in favour of arms-length, non-verbal communication.
Yet a few months into the pandemic and with time under their belts to assess the impact of telehealth, many GPs believe the rise of virtual consultations has resulted in fragmented care, a decrease in practice revenue, and an unwelcome focus on profit over patient outcomes.
The latest findings from an Ekas survey of GPs unearths an underlying concern that the rise of some telehealth services could undermine the fundamental goal of local practices: to deliver quality care tailored to individual patient needs.
Profit v patient care: the impact of virtual consultations
85% of those surveyed say they think telehealth is here to stay – but despite this prediction, more than two thirds (70%) believe the increase in instant consult technology has had a negative impact on overall patient care.
Topping the list of their concerns is the effect on continuity and consistency of care. When asked if the availability of instant consult services has resulted in fragmented care as patients move between in-person and virtual consultations, 87% agreed it had. And while 46% of practitioners agreed the new technology provides patients with more easy-to-access services, 75% say these services are driven by profit over improving patient care.
One practitioner explains it is “vital that fragmentation of care is not encouraged” and that “new patients understand that telehealth assessment is suboptimal and limited”.
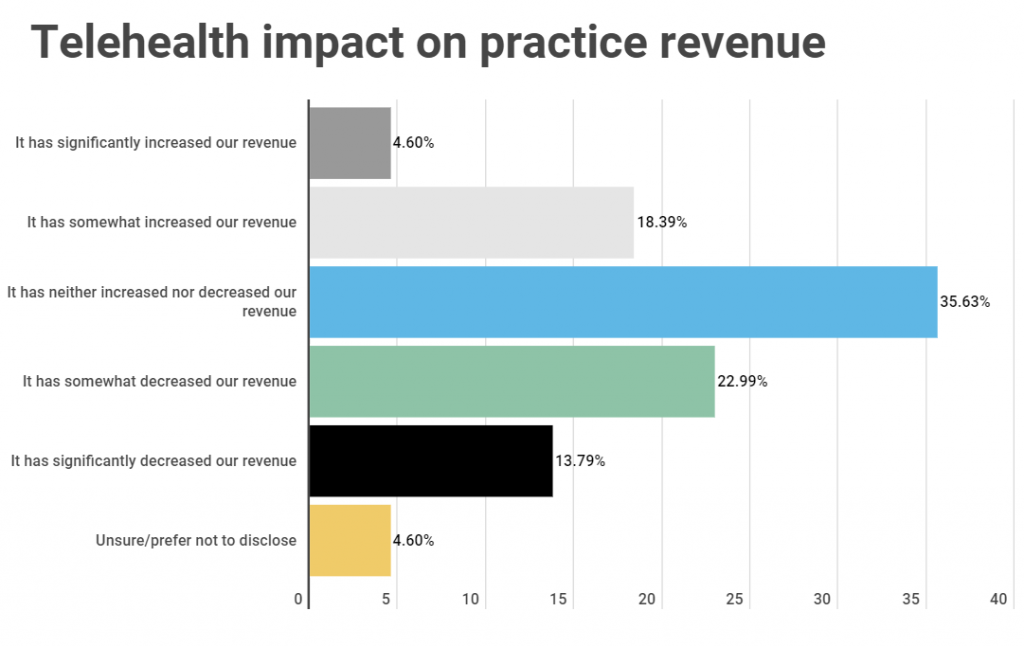
Over a third (36%) of practitioners say the launch of telehealth services has had no impact on practice revenue, while 37% believe it has had a negative effect on revenue.
So, how did we get to this ‘new normal’?
The COVID era has seen a huge rise in the takeup of convenience-led technologies designed to make our lives easier. Australian online shopping orders set a new record in April 2020, Zoom’s corporate customers have quadrupled YoY – so isn’t healthcare just the next logical service to be ‘virtualised’?
The explosion in telehealth consultations would suggest the move to virtual appointments was inevitable. 92% of practitioners questioned in the Ekas poll say their practices now offer telehealth services, with 90% of these services launched during COVID. That’s a huge shift for a profession built on face-to-face appointments and physical examinations.
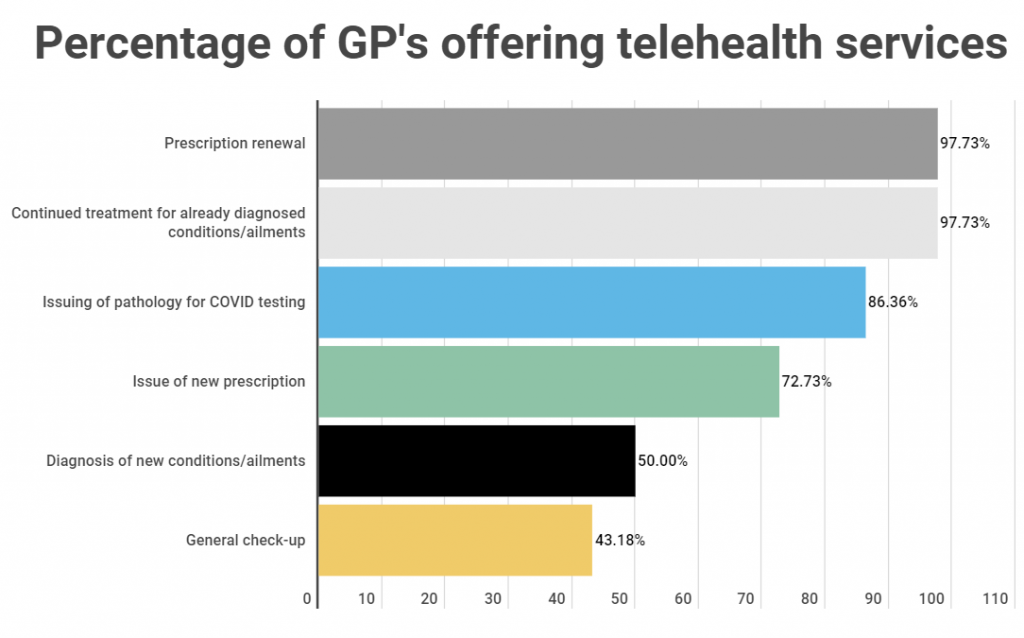
The most popular services offered via telehealth consultations include prescription renewal (offered by 98% of practices), continuing treatment for pre-diagnosed conditions (98% of practices), issuing pathology for COVID testing (86% of practices), and issuing new scripts (73% of practices).
When telehealth works
If there’s anything we can be certain of in these uncertain times it’s that more change is coming. The unprecedented second wave of cases in Victoria and NSW shows just how volatile the current health crisis is. So with telehealth ‘here to stay’, how can practitioners best use it as a force for good? And in what situations does it make sense to choose telehealth over in-person appointments?
88% of those surveyed believe telehealth services should be offered only through a patient’s regular practice or practitioner, which could help improve continuity of care and reduce some people ‘shopping around’ for appointments.
One practitioner explains telehealth “is convenient and useful during COVID, [and] may have certain benefits post COVID, especially for stable/regular patients, and for simple things like repeat prescriptions, referrals to specialists or pathology”.
There was also a general consensus among GPs that telehealth definitely has a role to play for those patients who are physically unable to visit a surgery. 74% of those polled say telehealth should be used some of the time for patients whose conditions prevent them from attending in person, and 23% believe telehealth should be used all the time in these cases.
In addition to this, 90% of practitioners say telehealth should also be used at least some of the time when it comes to managing existing patient care. 92% believe telehealth should be used at least some of the time for script renewals, and 68% say it should be used at least some of the time for new prescriptions.
Perhaps unsurprisingly, the case for telehealth usage is less positive for diagnostic consultations where physical examination or discussion is usually needed. 56% of practitioners believe it should not be used to diagnose new conditions.
They were also less willing to embrace the new technology for issuing referrals, particularly when it comes to new patients with 71% saying they do not think telehealth should be used to issue referrals to new patients.
More than three quarters of practitioners polled (76%) say they are worried about abuse when it comes to instant script services, and 37% are so concerned about how the current technology is being utilised that they do not believe it should continue post COVID.
In addition to this, 66% think instant script services focus on profit-driven models rather than patient care – a sentiment that offers food for thought for future healthcare innovators when it comes to the next iteration of telehealth services.
What next for telehealth 2.0?
Local patient care has adapted rapidly to the biggest societal shift in a generation. They say necessity is the mother of invention, and telehealth – borne from necessity at a time when the pandemic has almost paralysed society and the economy – has fulfilled its role of delivering personalised services to an isolated population.
Yet when the pandemic stabilises and the dust settles, what will be the role for telehealth then? As the first two decades of the millennium have taught us, once a new technology takes root it’s very hard to go back. And in an era when we’d rather tire out our thumbs sending texts and emojis than speak to someone in person, there’s a certain appeal to being able to get a script or a routine check-up without disrupting your day.
But unlike retail, food and (to a certain extent) the fitness industries, where in-person contact is no longer mandatory for the service to function, healthcare presents a trickier problem for technology to solve. It’s hard to evaluate a patient’s physical, mental and emotional needs via a virtual consultation. “Telehealth is never patient-centric,” explains one practitioner. “It is Uber medicine.”
Practitioners must continue to be a major voice in the debate around future healthcare innovations to ensure telehealth 2.0, whatever form that takes, evolves into something that truly transforms the delivery of patient care services.
Key findings
92% of practitioners say their practice offers telehealth services.
90% of practices launched telehealth services during COVID pandemic, 9% of telehealth services launched pre COVID.
85.11% of practitioners believe telehealth is here to stay.
88% of practitioners believe telehealth services should only be offered through a patient’s regular practice or practitioner.
70% say the increase in telehealth services have had a negative impact on managing patient care.
The most popular services offered via telehealth consults were prescription renewal (98%), the continuation of treatment for pre-diagnosed conditions/ailments (98%), and the issuing of pathology for COVID testing (86%)
23% of practitioners say telehealth has increased practice revenue, 36% telehealth has neither increased nor decreased practice revenue, and 37% say practice revenue has decreased since launching telehealth services.
87% agree it results in fragmented care as patients move between their regular practice and that of telehealth services.
46% believe it provides patients with more easy to access services.
75% agree services are generally driven by profit and not the patient.
The Ekas telehealth survey polled 153 GPs practising in Australia.
