When it comes to headlines about health issues, the topic of mental health has historically been under-reported in the media.
Often when mental health does make the news it is because there has been a tragedy or a perceived failing – or someone has fallen through the cracks in the system.
Is this reticence because society remains unwilling to treat mental health issues the same way it would any other disease or illness, or because of a lack of education and understanding about the impact of mental health conditions on patients and their families? Potentially both.
However, public awareness appears to be shifting. Since the Covid pandemic hit and the modern way of life changed in a way very few of us could have ever foreseen, mental health has never been more important nor more openly discussed.
Covid-19: changing the mental health conversation
While the initial focus of governments and health authorities was to squash or limit the spread and impact of the virus, the widespread effect of lockdowns, reduced liberty, job losses and economic instability is having a real and ongoing impact on a significant proportion of the population. Recent research undertaken before the recent lockdowns revealed almost 1 in 5 Australians reported ‘high or very high levels of psychological distress’. (https://www.theguardian.com/world/2021/jul/14/covids-mental-health-toll-one-in-five-australians-report-high-levels-of-psychological-distress)
Prioritising mental health has now become a key focus on a state and commonwealth level, particularly during the most recent extensive lockdowns. The NSW and federal governments have recently launched a joint $17m package to offer access to wellbeing and mental health support and increased access to services. https://www.health.nsw.gov.au/news/Pages/20210714_01.aspx
This is a vital and necessary step to provide support during the current crisis, but what can be done to ensure mental health remains high on the national agenda long after society opens up again?
We spoke to a select group of psychologists working with children and adults under 30 – two of the groups most acutely affected by the current restrictions – to get a deeper understanding of how authorities can help improve access to mental health services, and how to remove barriers to addressing mental health concerns.
Taking the first step in seeking help
Not everyone who needs mental health support is willing to make the leap and talk to someone. In fact, choosing to see a psychologist can often be the step people take when they feel they have exhausted their own coping strategies.
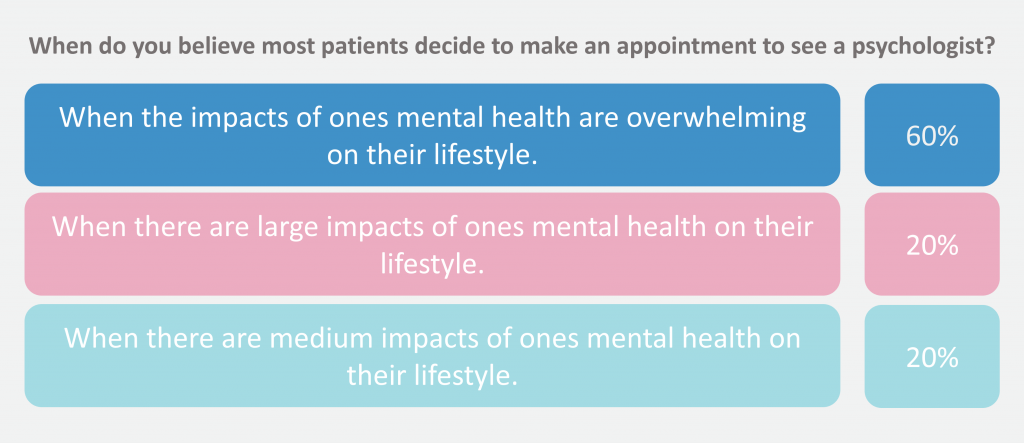
All psychologists we spoke to agreed that patients make their decision at the point when their mental health condition is having a medium to significant impact on their daily lives, with 3 out of the 5 practitioners saying they believe most patients decide to make an appointment when the impact on their lifestyle is ‘overwhelming’.
The point in time when patients actually seek help differs significantly from when the majority of psychologists professionally believe they should book their first appointment. 83% said the best time to get a mental health check is when there are small to medium impacts on a person’s lifestyle.
So why the reluctance?
Despite society evolving to be more open in its discussion of mental health issues, the clinicians polled believe there is still a stigma associated with seeing a psychologist, which prevents people who require help from reaching out. 80% say this is the case some of the time, and 20% say this is the case most of the time.
One psychologist commented: “The shame and stigma is embedded at a societal level. A cultural shift is required.” While she accepts it does feel like this shift is starting to happen, she believes a “lack of access to services perpetuates difficulties”.
A psychologist working with children and young adults explained that although “some older generations hold beliefs that acknowledging mental health concerns is a negative thing,” she doesn’t see this among the patients she works with themselves.
The psychologists also cited the cost associated to access help, feelings of shame and lack of awareness of self and support resources as being the top reasons patients may be unwilling to seek help.

‘Mental health care is a legitimate and needed use of the health system’
Perhaps one reason mental health has not received the focus it deserves is because it has historically been seen as separate from physical health conditions. However, with a rising understanding and acceptance of more holistic healthcare approaches, authorities are recognising that mental and physical wellbeing are intrinsically linked.
When asked why it is vital that those needing mental health support are given access to it, one psychologist commented: “Mental health care is a legitimate and needed use of the health system. Mental health has impacts on physical health and vice versa.”
So what more can be done to ensure those who require access to mental health services get the support they need?
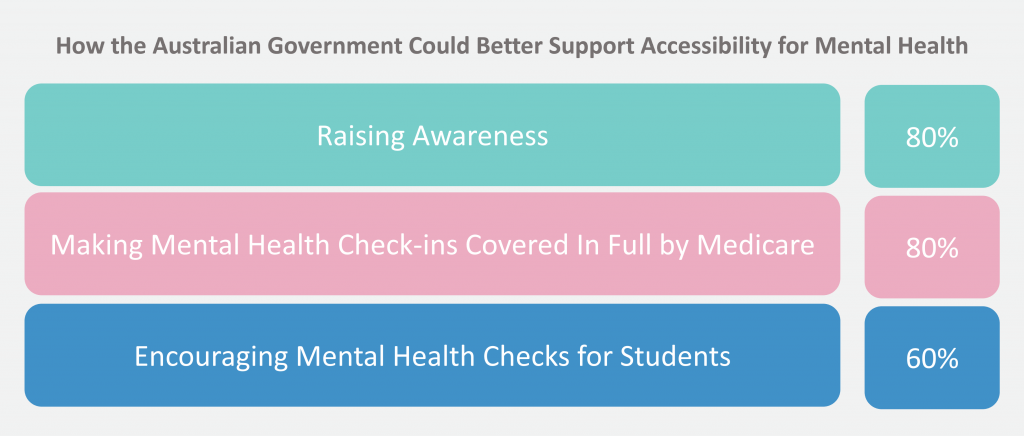
All of those polled agreed the Australian government should support access to mental health services more. Raising awareness of available services and making mental health check-ins covered by Medicare were the top two strategies preferred by psychologists.
Three out of five also believed encouraging mental health checks for young people could be an effective strategy in helping patients address issues early on.
The intergenerational effects of untreated mental health problems
While yes, the Covid-19 pandemic is shining a light on mental health issues, the long-lasting impact of the current lockdowns may be felt for many years to come. This is why, when the dust settles on these long months of lockdown and life returns to its new normal, the conversations around stress and mental wellbeing need to continue well beyond the time life opens up again.
The toll of untreated mental health issues not only affects the patient, but it has the potential to be felt by future generations.
“There are large economic and societal impacts of untreated mental health difficulties,” commented one respondent.
Another explained that if underlying conditions are not addressed: “Lifelong mental health patterns are not resolved. These are role-modelled onto future generations.
“Without our mental health we cannot be 100% physically fit.”
Key findings:
- 83% of psychologists polled believe the best time to get a mental health check is when there are small to medium impacts on a person’s lifestyle.
- 100% believe the Australian government should support access to mental health services more
- 100% say a therapeutic alliance between patient and practitioner is very important in allowing for successful therapy
- 60% believe most patients book their first appointment when they are at the point when the impacts on their lives are overwhelming
Ekas spoke to a select 5 Psychologists on its panel Medical Opinion Leaders in August 2021.
