We often associate eating disorders as a problem experienced by youth, and it is true that commonly, these disorders are triggered during adolescence. However, as a serious psychological condition, eating disorders can significantly affect sufferers throughout their life, and the experiences of older sufferers is less often considered.
In a recent EKAS research poll, we surveyed sufferers of eating disorders aged between 18 and 75, finding heartbreaking insights into the triggers, daily life and ongoing struggles of their illness, as well as perspectives from sufferers on how to move forward or support someone you know who is affected.
One in ten Australians suffer from an eating disorder…
The National Eating Disorders Collaboration (NEDC) estimates that around one in ten Australians suffer from some form of eating disorder. The most commonly recognised eating disorders are Anorexia Nervosa (characterised by placing severe restriction on food consumption), Bulimia Nervosa (sufferers eat or binge eat, and then purge the food they have consumed) and Binge Eating Disorder (sufferers regularly consume large quantities of food in a short time period).
Rather than being health-conscious or considered as dieting issues, eating disorders are mental illnesses, and with each of these disorders comes detrimental psychological burdens that affect many aspects of the lives of sufferers and those around them. One respondent described the impact on relationships the disorder has had, “I’ve lost a lot of social connections and it has also impacted family life in a negative way”.
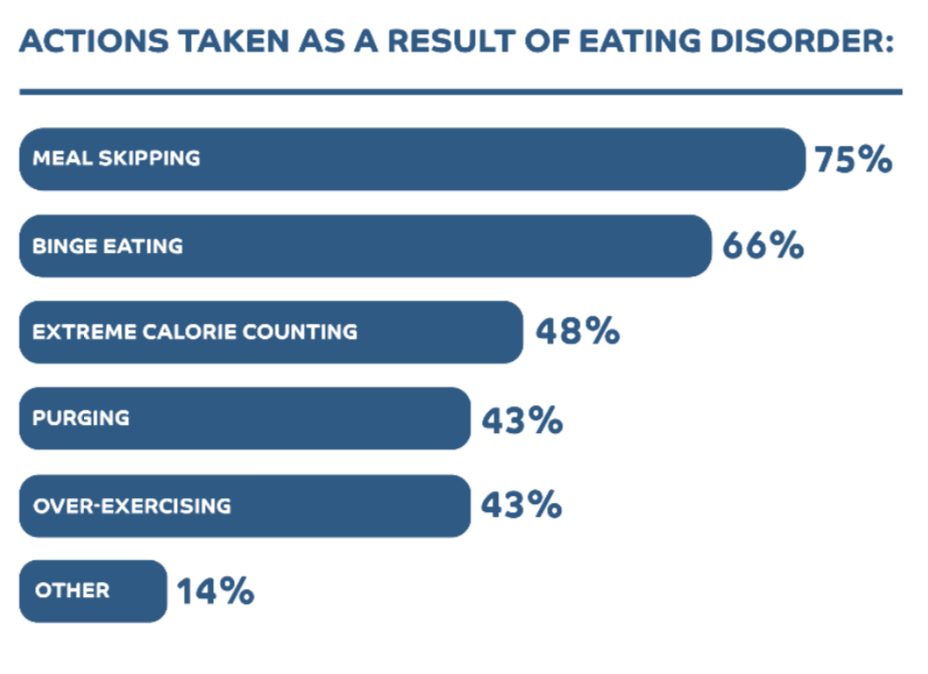
Respondents to the survey listed the types of actions they have taken as a result of their eating disorder, the most common being meal skipping (75%), binge eating (66%), and purging (43%). Purging includes acts that remove food/calories from the body, such as induced vomiting, taking laxatives, or fasting excessively. Often, behaviours can also be hidden under the guise of fitness or health consciousness, with sufferers also reporting used excessive exercise (43%) and extreme calorie counting (48%).
Not just an adolescence issue.
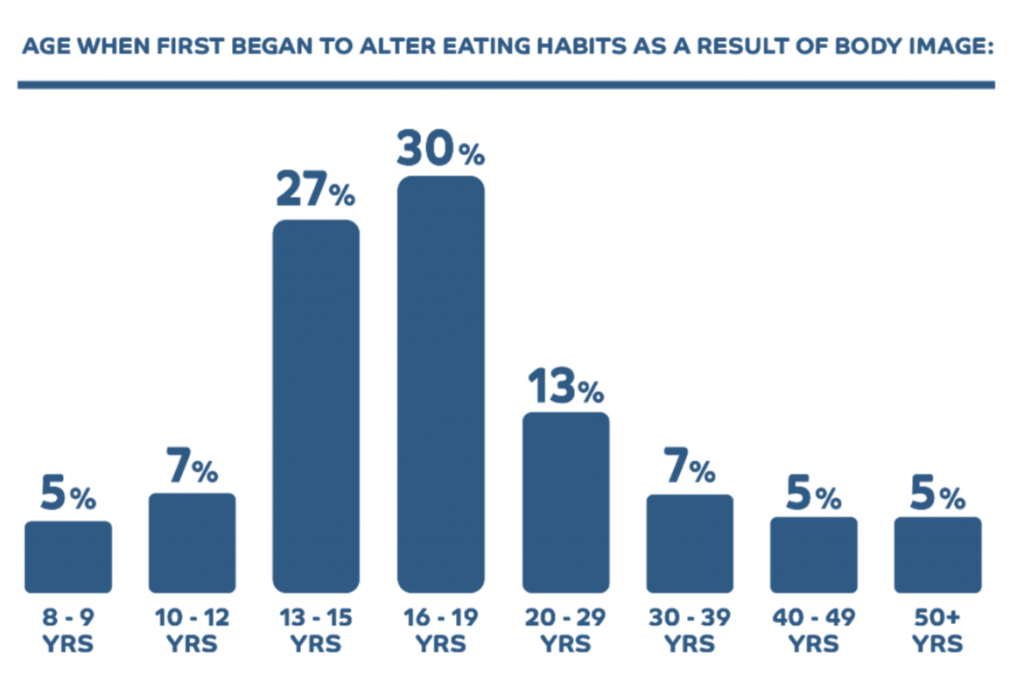
Of the those surveyed through our poll, the most common type of eating disorder respondents suffer or suffered from was Binge Eating Disorder (52%), followed by Anorexia Nervosa (43%). As is commonly the case in the development of eating disorders, the majority of respondents were in their teens, or younger, when they first started to alter the way they ate as a result of body image (70%), and of these, 18% were under the age of 12.
For the significant remaining portion of the group, the tendencies that led to their disorders developed in adulthood, either in their twenties (12%), or older (18%). To recognise the signs of these issues, it is vital to be aware that eating disorders can affect people of all genders, cultures and ages.
The possibility of recovery…
Regardless of the age at which the condition was triggered, these mental illnesses can become lifelong afflictions. Whilst the majority were struggling with these conditions as children or teens, only 42% of sufferers started to receive help during this age period. The majority started receiving help as adults, in their twenties (25%) or older (33%).
Of the respondents surveyed, only 20% considered themselves recovered enough to declare they are no longer living with the eating disorder. The remaining are still suffering – either currently living with their eating disorder (40%) or feeling they have distanced themselves from the eating disorder but need to be mindful of triggers (40%). For those still living with it, their life may be heavily consumed by the effort of the symptoms or trying to manage them – “It takes up part of my mind constantly, [it’s] hard to focus, I have to actively work on it every day” one respondent explains.
Where does it begin?
There are many unique factors that play a part in the formation of an eating disorder. Respondents most commonly described the main triggers which led to their disorder being psychological, such as another underlining condition like anxiety or depression (72%), or social factors (53%). One sufferer described their triggering into the disorder as “severe body image distortion and social pressure to look a certain way”.
Of course, body image is a core trigger for many sufferers, and is a complex social construct that can start to impact negatively, even when a person believes their focus is on health. This respondent described how their trigger was a result of a positive change to their health; “I lost weight and lots of people commented on how great I looked and I got more attention. Then I started to get nervous about putting on weight and it escalated from there”.
Another common misconception about eating disorders is that they are always rooted in body image. Again, whilst this may be a common cause, it’s important not to assume this as always the case, as succinctly expressed by one respondent, “Not all disordered eating has to do with body image. It isn’t in my case. It is a direct result of trauma and depression”.
Seeing the world through the eyes of an eating disorder…
When you consider that food and eating are a core function in everyday life, as well as a significant factor in how we socialise – it’s hard to imagine navigating life with an eating disorder. “It affects every aspect of your life, because food and weight conversations are everywhere”, one respondent describes.
Others expressed feelings of constant worry, exhaustion, or numbness, and the fact of having to miss out on aspects of life to avoid their triggers – “I feel like I can’t function as a normal person. I’m either always hungry, or sick from bingeing – there’s no in- between. I feel like I can’t engage with any activities where there will be food”.
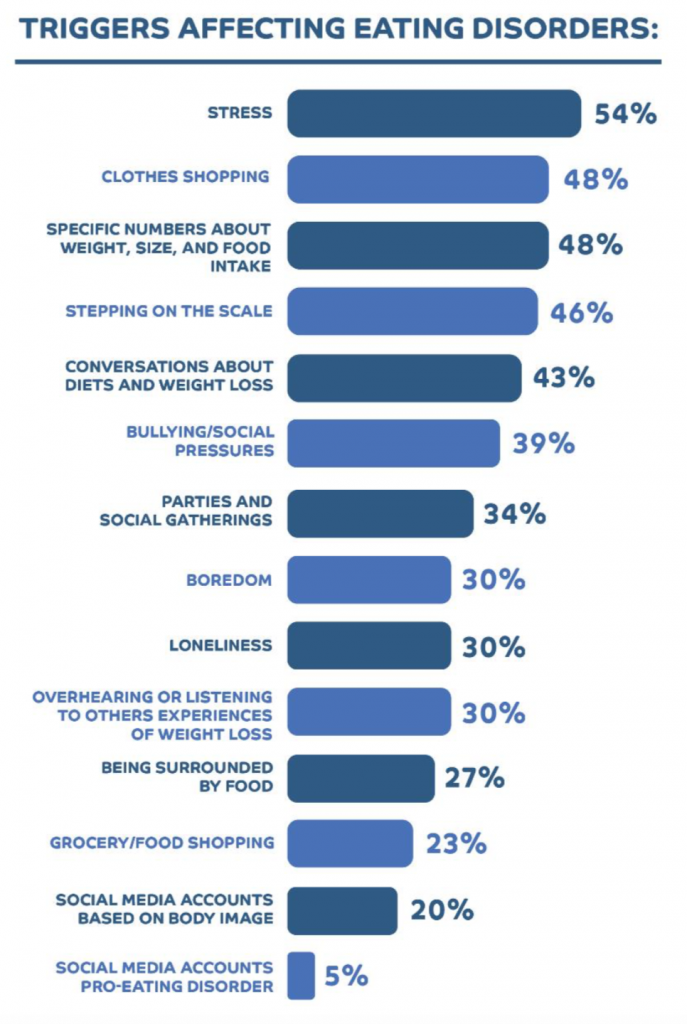
When asked what were the most common triggers which affected their eating disorder, respondents indicted stress as the most significant (54%). The next most common trigger was clothes shopping (48%), followed by specific numbers about weight, size, and food intake (48%), stepping on the scale (46%) and conversations about diets and weight loss (43%). Sufferers face a difficult task in avoiding such type of conversations in Australia’s increasingly popular health and fitness focus, as well as the part that social media plays in increasing the prevalence of these topics.
The terrible trap – eating disorder accounts on social media.
For all users, social media can have a detrimental effect on body image. The effects of the wrong combination of influencer, fitness, clean-eating or diet accounts can play a devastating role in negative body image, but for those already suffering from an eating disorder an additional trap lies in another type of account.
Pro-eating disorder accounts, commonly found on Instagram, promote eating disorders such as Anorexia Nervosa as an aspirational lifestyle. Providing tips and “inspiration” to achieve the goals of the eating disorder, accounts sometimes even describe themselves as coaches.
Of the sufferers we surveyed, a small portion have engaged with social media accounts or sites such as these (9%). They described having had a complex relationship with the accounts, one retelling their
conflicted view – “[They] feed my disorder but I also crave the images I see” – while another explained that it does feel like they provide a sense of support – “They provided understanding and made me feel like I wasn’t alone. It wasn’t with the intention of making myself more ill, but about finding people who understood”.
Learning to see food as fuel, not as fear…
We asked what steps sufferers have taken to try to manage the triggers for their eating disorder, and answers included removing the types of toxic social media pages mentioned above, if not ceasing social media use all together, as well as removing calorie counting apps.
In terms of supporting a friend or loved one who is enduring an eating disorder, one respondent offered this thoughtful advice; “To try and encourage them wherever possible. Tell them that they are worthy and deserving of food. I found it helpful if someone chose to eat something, because it made me feel like I could also eat”.
After asking what advice sufferers may give others finding themselves dealing with eating disorders, there were many words of encouragement to seek professional help, not to feel ashamed and find support in friends or family. As this respondent advised, “Take it a step at a time and reward yourself for taking the one step”.
If you or anyone you know needs help with an eating disorder, contact:
- Butterfly Foundation on 1800 33 4673
- Lifeline on 13 11 14
- Kids Helpline on 1800 551 800
- Beyond Blue on 1300 22 46 36
- Headspace on 1800 650 890
Ekas Surveyed 55 members on it’s panel Apple A Day in November 2020 who are living with an eating disorder.
