2020 isn’t quite over yet, but already it’s poised to go down in history as one of the most challenging years in modern times. With a global pandemic and its subsequent fallout coming on the coat-tails of the most catastrophic bushfire season ever recorded, it’s not an exaggeration to say this year has brought unprecedented hardship to many Australians.
While most of the population have had to contend with food shortages, social distancing and restrictions on the liberties they have always taken for granted, some Australians have been hit even harder.
2020 has been a particularly worrying time for elderly people and patients with pre-existing health conditions. Those with asthma, for instance, have had to contend with not only the oppressive smoke from the bushfires at the start of the year, but also the uncertainty around COVID-19 and its potential impact on their health.
The National Asthma Council says that there isn’t enough evidence yet to know how COVID-19 affects people with Asthma, however it advises those with respiratory conditions to take extra care. While further studies and specific information on COVID and asthma is still pending, the known impact of the virus on the respiratory system still raises anxieties for those with conditions such as asthma.
Access to medication supplies limited; fears rise over virus exposure
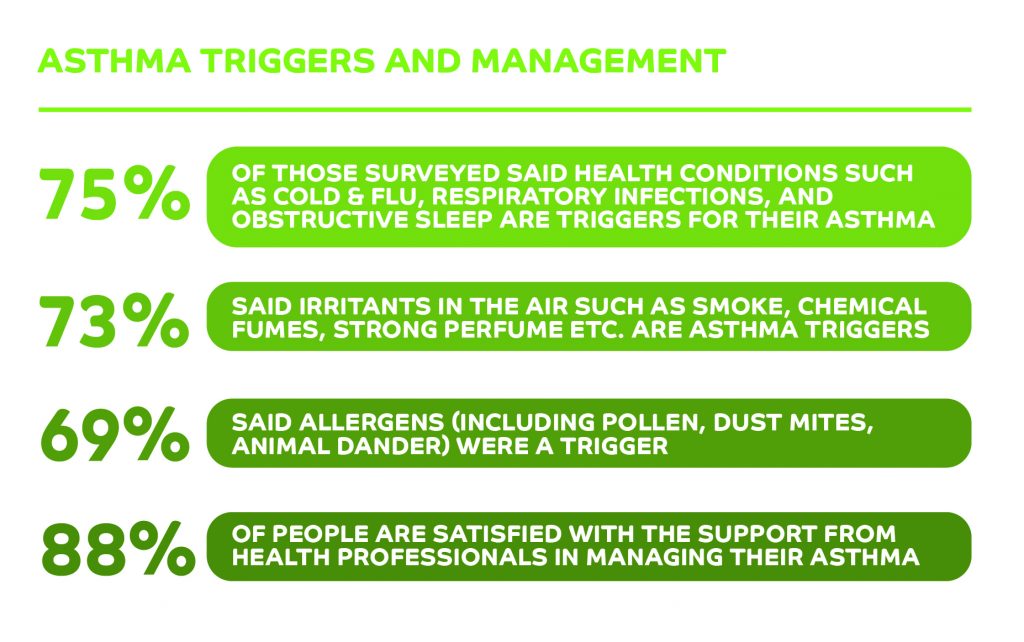
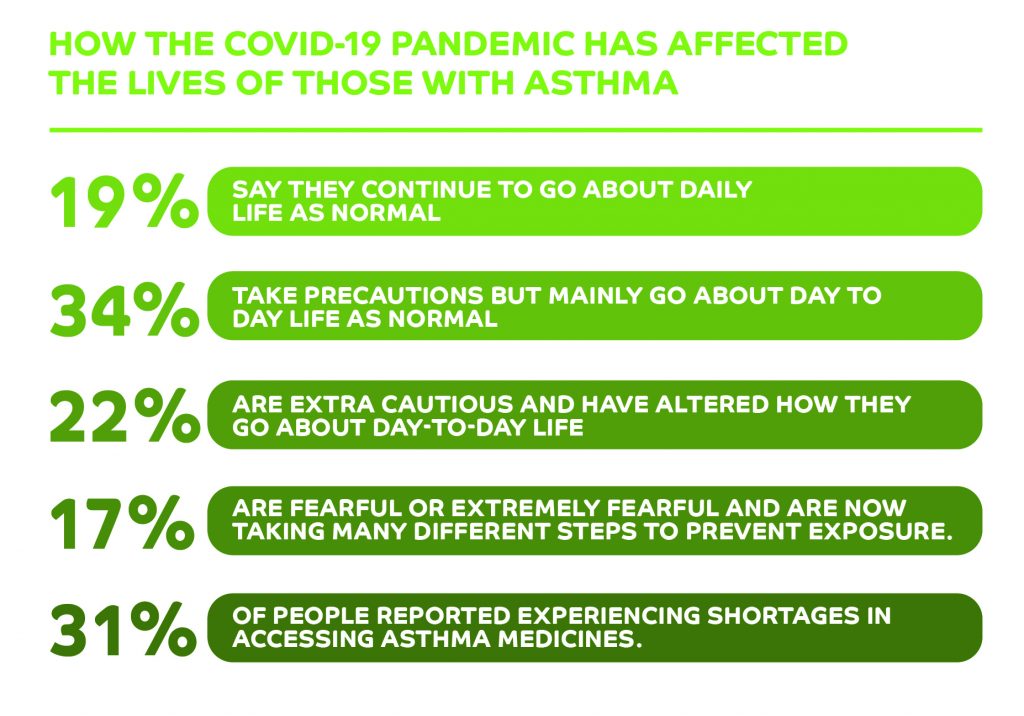
An Ekas survey of people with asthma and carers of people with asthma found 22% of those polled are now extra cautious and have altered how they go about their day-to-day life since the pandemic started, and 16.5% say they felt fearful or extremely fearful and are now taking additional steps to prevent potential exposure to the virus.
The pandemic also caused medical supply issues that patients could have never foreseen. 31% of respondents reported experiencing shortages in accessing asthma medicines at the start of the crisis.
To get a deeper understanding of what 2020 has really been like for those with asthma, Ekas’s Panel Manager, Jessica Farrow, sat down with a member of our patient panel, Apple A Day, to discuss the day-to-day challenges she faces.
Jane was diagnosed with asthma while still in primary school. With a family history of asthma, Jane has grown up managing her health, and now is raising her 7-year-old son, who has also been identified as having probable asthma.
Understanding a childhood asthma diagnosis
Jane was diagnosed with asthma when she was just seven years old, the same age as her son, who is now considered borderline asthmatic. He cannot be diagnosed formally due to his age and the fact he is living with other sensory issues. While Jane’s asthma is considered mild, she is still required to use a preventer and reliever.
Jane recalls her early memories of being diagnosed with asthma and learning that her mother and grandmother were also asthmatic.
“I remember being told that that I’m an asthmatic,” she says. “I remember wheezing a lot, especially in wintertime because of the wood smoke in the area I lived in. Running around at school I’d be short of breath.”
Jane recalls the initial test being performed alongside an allergy test at a specialist centre. “I have more memories of the needles that the actual test, but I do remember the doctor saying I had asthma and it was mild.”
Adapting daily life to known asthma triggers
To be given a diagnosis at such a young age meant Jane had to make changes to avoid known triggers. And while the asthma was not severe enough to result in asthma attacks, it was still uncomfortable for a young child who just wanted to be able to play with friends and do things all her peers were doing .
Now an adult, Jane relies on her Ventolin. Any changes to the seasons can be triggers, particularly when it has not rained for a while and the wind picks up dust and allergens in the air.
“I always have my reliever (Ventolin) with me because even if I’ve had my preventer it still affects me,” she says.
“The wind direction affects it as well… and the wind picks up everything… [especially] if we go for a walk somewhere like a botanical garden.”
Jane has spent much of her life adapting to living with asthma and taking preventative steps such as checking the weather and conditions before she plans for the day ahead. Changes such as these are now just a part of her daily routine in reducing her and her child’s risk of exposure to asthma triggers.
Raising a child with probable asthma
Jane’s own experience with asthma meant she and her partner were attuned to the signs to look out for. So when her son presented with similar symptoms, such as complaining his chest hurt while running and wheezing during changes of season, she knew she also needed to take him to get checked.
She says: “He also gets the same thing that I do where the bottom edge of my lip turns a bit blue.
“That was something that my partner actually noticed and said we should get checked out because he did have croup a lot in the first 2-2.5 years of his life. I think we took him to the hospital six or seven times with croup.”
Explaining the importance of asthma medication to a young child can be challenging, but Jane and her partner have found the best approach is to go through the process step-by-step, offering reassurance that his preventer is there to assist him with breathing.
“We just try to say ‘we know it tastes yucky but it needs to be done to help you breathe better’, says Jane.
“We explain that if you don’t have it now you might have to go to hospital a little bit later. Because you may be struggling too far that we can’t help you.”
The impact of the catastrophic bushfires on people with asthma
73% of people polled in our recent survey said irritants in the air such as smoke and chemical fumes can trigger their asthma. These findings have serious and very real implications for people living with asthma, particularly those in areas affected by the most recent catastrophic bushfire season.
Jane lives in one of these areas and spent much of her summer indoors as there was a fire burning between two nearby towns.
She recalls: “I didn’t see the sky in about five months, so with all the smoke around we kept the house closed up and I limited my time outside”.
“I didn’t leave the house very much at all, which was not good for my mental health, but if I left the house I couldn’t breathe so it was kind of ‘I’m damned if I do I’m damned if I don’t’.”
The ever-present smoke in the air was also affecting Jane’s son, who found it difficult to breathe. He was taking his preventer medication (Flixotide Junior) twice a day, then having Ventolin when he went to school or at home. The school supported Jane and her son in his needs and he was particularly encouraged to take it easy at school and find a teacher if he was experiencing trouble breathing.
The mental and emotional toll of bushfire season
As well as the obvious health implications of poor air quality on those with asthma, the stress of being confined indoors for prolonged periods of time and having to make stay-or-go decisions had a significant emotional and mental impact. Jane describes how it felt to be in this situation which was all too real for many Australians.
“Fire scares me and at one point our house was right in the line of the fire,” says Jane. “We made the decision to evacuate, which was hard because I wanted to be with my family”.
“I wanted my partner to come with me, but he stayed because his mum was here. I had the anxiety of leaving and the anxiety of him staying. It was just a bad time”. Jane continues to highlight the moment she left with her son and not knowing when exactly they would be able to return home, but knowing she needed to make this decision as her and her sons ability to breathe in the area worsened.
“Thankfully it turned around and went back on itself so it burned itself out in our area.” Others weren’t so lucky to have their home saved.
COVID-19 and asthma: medication shortages fuel panic
Just a few short weeks after the worst of the bushfire season was over, asthmatics faced another, unforeseen challenge: the arrival of COVID-19 in Australia.
The virus not only put those with asthma on high alert – people with pre-existing respiratory conditions are advised to take particular care to avoid potential exposure – but it also prompted medication shortages.
Jane reports going three to four days without her preventer because the pharmacies in her area didn’t have any supplies left. As others overstocked to ensure access, some were left with none.
“I actually had to go without and I was relying heavily on the Ventolin at that point,” she recalls. “We’d been looking for about a week before I knew I was going to run out, but it took us about a week and a half to actually find it”.
“I was actually starting to panic because I didn’t have much Ventolin either.”
When Jane finally managed to get the medication she needed, she says it was a huge relief for her whole family, particularly her partner and her son, who no longer had to watch her lips turn blue as she struggled to breathe.
The new normal
At the height of the pandemic, Jane and her family barely left home. They home-schooled and did Tafe study remotely, only venturing out when absolutely necessary.
Now cases across NSW are low and life is slowly returning to a version of normal but for many people, the impact of COVID remains. Jane says the virus has changed her approach to daily life and managing her asthma.
“Since running out of the preventer I make sure that I have more than a week’s worth left,” she explains. “I make sure I have at least 14 puffs left on my Seretide inhaler when I buy another one”.
Because of her asthma, Jane finds wearing a mask difficult. But she has implemented other measures to help minimise the risk for herself and her family.
“I did try [a mask] for about half an hour and I couldn’t breathe… It was rather anxiety inducing for me, so I just maintain social distancing, and sanitise my hands regularly.”
“When we do the shopping, we try to do it mainly around 6-7-o’clock at night because there aren’t as many people at the shopping centre. Or only one of us will go and grab a couple of things when we need them so that we’re not all going out.”
While Jane hasn’t heard of any new reported cases in her area, she now has a plan in place should cases in the area occur, which includes having the right amount of medication on hand, self-isolating and has already spoken to the school about reverting to home-schooling again for her son if necessary.
Jane shares her thoughts on what is important to be ready and recommends, having enough preventers and relievers so you do not run out is vital. And while this doesn’t involve panic buying supplies, it does mean having back-up medication for when you need it.
She also believes staying present, having friends or family to talk to, and not trying to plan too far ahead can help with the mental load of managing a respiratory condition during the pandemic.
“I’m not watching any news, I’m trying to take it day by day at the moment,” she concludes. “Having someone to talk to is always good, even if it’s just to unload what’s in your head.”
Key findings:
Jane’s name has been changed to comply with our member’s privacy agreement. This interview was conducted in September along with our survey of 117 asthmatics to produce the findings in this article.
