The ways patients interact with GPs has changed dramatically in 2020. The COVID pandemic has made new consultation options such as telehealth appointments and community testing facilities a new and necessary reality.
While these developments provide some time savings and convenience for patients at a time when our healthcare services face some of their toughest challenges in living memory, it prompts the question: what more can be done to drive greater efficiencies?
One concept gaining traction among academics, patients and healthcare professionals is a National Minor Ailment Scheme (MAS). Such schemes offer a formal referral pathway between community pharmacists and GPs or emergency departments, making pharmacies the first port of call for minor conditions such as colds, allergies, low-level gastro-intestinal complaints and back or menstrual pain. Where such schemes have been trialled, pharmacists assist patients in finding appropriate over-the-counter medication, offering advice and triaging cases to GPs or other service providers if required.
Although many MAS models exist overseas, and studies in Australia show there could be significant time and cost savings by formally introducing such initiatives here, awareness among pharmacists of the scheme is low.
Minor Ailment Schemes: the pharmacy profession’s view
A recent survey of pharmacists on our Medical Opinion Leaders panel found just 18% had heard about the recommendations to implement a national MAS in Australia.
Despite this, 93% of those polled believe it would be beneficial to pharmacists, patients and the healthcare sector as a whole.
“There are many benefits,” said one pharmacist. “[It] reduces GP and potentially emergency department visits that could be handled in a pharmacy. These savings could then be reinvested in other areas of the healthcare system.”
A University of Technology Sydney study supports this sentiment. It investigated the impact of evolving the role of pharmacists in community healthcare and found “clinical and economic evidence” an MAS would be successful in Australia.
Dr Sarah Dineen-Griffin, chief investigator of the study, said: “Patients seeking care from GPs and emergency departments with minor ailments cost the Australian health system between $511 million and $1.67 billion per annum. National implementation of a collaborative consultation service can alleviate pressure on the health system and save up to $1.3 billion a year.”*
Time and training key to MAS success
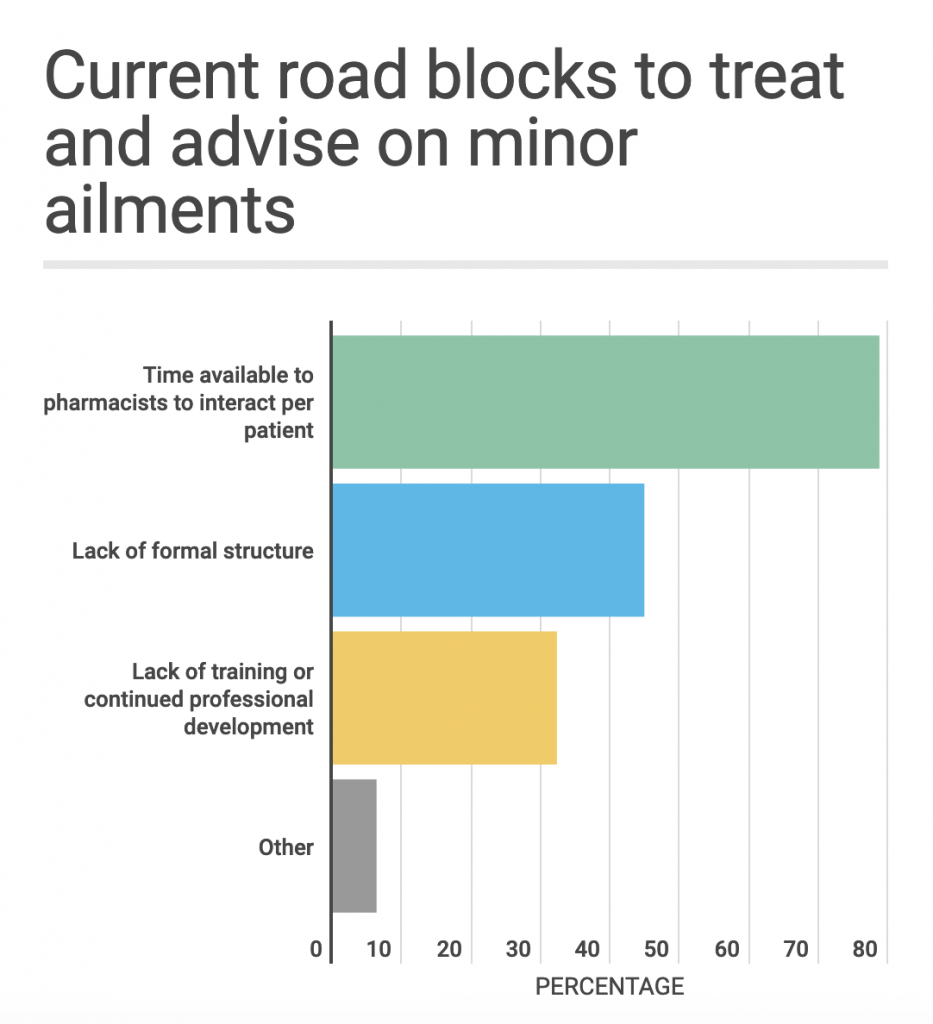
With a majority of practising pharmacists believing the scheme could have a positive impact, what are the barriers preventing its adoption?
Lack of time is the biggest blocker reported by pharmacists, with 79% saying this prevents them from currently advising on minor ailments.
Our survey reveals a high level of confidence among the profession when it comes to dealing with the most common minor conditions. 85% say they feel very confident in treating and advising on colds and flu, while 63% say they feel very confident in treating and advising on minor cuts and bruises.
There was also a strong feeling among respondents that they are already fulfilling many of the expectations of pharmacists working as part of a MAS. Almost three quarters (74%) of those polled believe they have the required training to support the implementation of a nationwide scheme in Australia.
Remapping roles in community healthcare
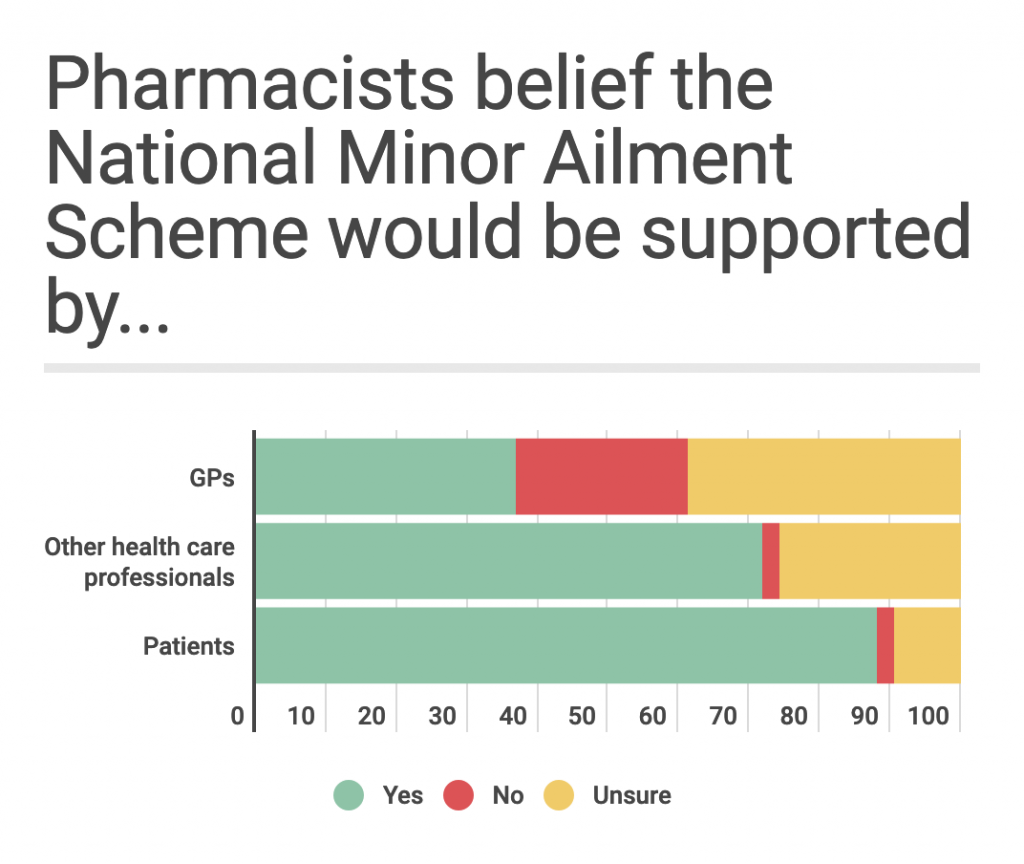
While support for rolling out a national MAS is high among the pharmacy profession, opinion is split over whether GPs would be in favour of the model. Only 37% say they believe GPs would be supportive of a national MAS, while 72% believe it would be supported by other healthcare workers and 88% think it would be supported by patients.
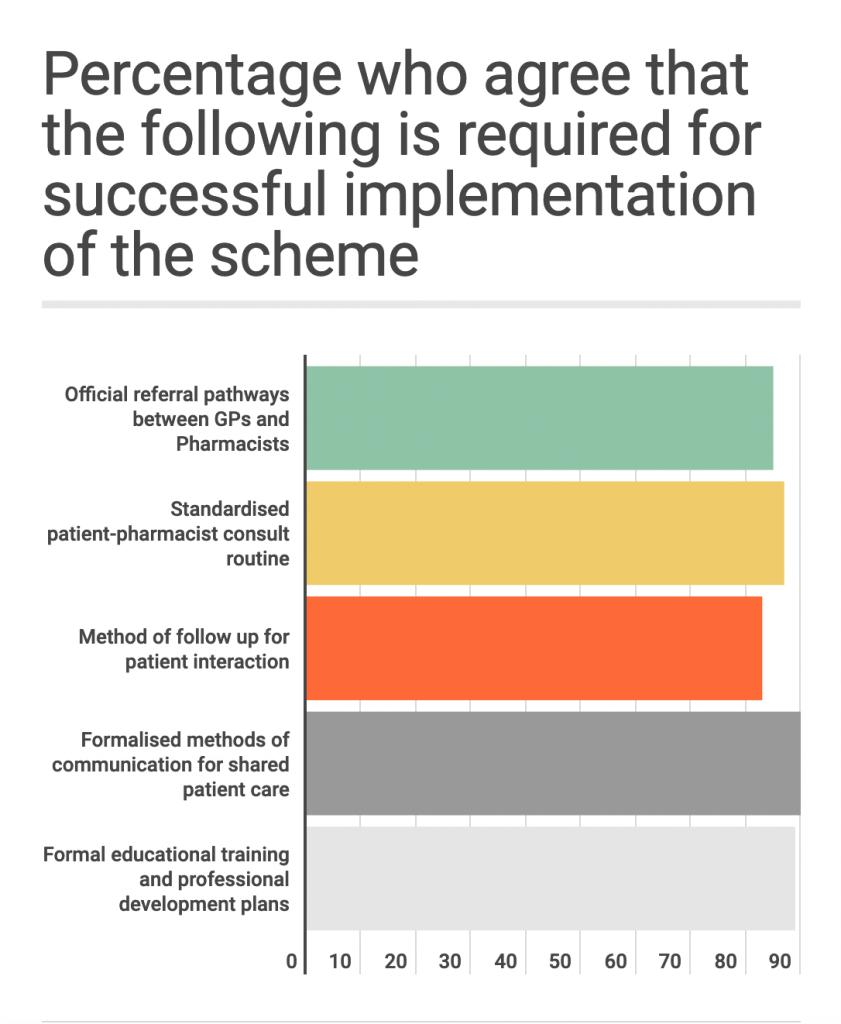
With doubt surrounding how much backing a nationwide MAS would have from all sectors of community healthcare, many pharmacists would like to have clearly defined roles so it is clear where their accountability starts and ends.
A majority of the pharmacists we polled believe a less ad hoc approach to pharmacist-patient consultations, together with an official referral pathway between pharmacists and GPs, are essential in facilitating such a major shift in community healthcare. A majority (90%) say official training and professional development plans and formalised methods of communication for shared patient care are vital for successful implementation of a MAS.
So could the widespread adoption of an MAS model in Australia become the norm rather than a trial for a select few? Pharmacists are already the first point of contact for patients hoping to bypass unnecessary GP visits for minor conditions, so it would be a logical progression for this consultation model to be standardised across the country.
Former Pharmaceutical Society of Australia President Dr Shane Jackson said during his tenure: ‘There’s no doubt that pharmacists actually save healthcare costs by dealing with common illnesses that don’t require a visit to general practice or the emergency department (ED).’
Many practising pharmacists see a nationwide MAS as an opportunity to collaborate more closely with GPs and other healthcare professionals to alleviate bottlenecks in the system, allowing doctors to focus on those patients with more serious conditions.
It also has the potential to attract more pharmacists into the profession with the promise of further career development and a clearly defined role in the provision of community health services. And, as 2020 has proven, anything that frees up time for those working on the front line of healthcare, is surely worth pursuing.
“[I’m] very hopeful that it comes to fruition.” said one pharmacist on our panel “[It] would be a welcome professional addition to pharmacy’s contribution to improved healthcare.”
The Medical Opinion Leaders survey polled n=259 pharmacy professionals in October 2020.
Key findings
18% of respondents had heard of recommendations for the implementation of national minor ailment scheme
93% agree or strongly agree it would be beneficial to pharmacists,
74% believe they are trained to be able to support the implementation of such a scheme
37% of those polled believe the scheme would be supported by GPs, 25% thought GPS would not support it, and 39% were unsure.
88% of those polled believe the scheme would be supported by patients, 2% thought patients would not support it and 10% were unsure.
