As parks and beaches once empty now erupt with small groups enjoying spring picnics, there’s a palpable sense of change in the air. After more than 18 months of COVID-19 lockdowns and restrictions, the pathway to freedom is becoming clearer for many Australians.
While it’s heartening to watch the cheerful scenes of friends and families enjoying the simple pursuits of outdoor socialising they’ve been denied for so long, with this cherished freedom comes rising concerns about what life will really be like post pandemic.
The hiatus from daily life hasn’t simply forced a hard stop to many activities’ society has taken for granted – attending schools, restaurants and workplaces, entertaining family and friends, participating in sport and leisure activities – it has also pressed pause on some essential medical check-ups and appointments. In pre-COVID times these appointments would be helping push patients through the system, enabling prompt diagnosis and treatment for other – sometimes chronic or life-threatening – health conditions.
Much has been made of the initial vaccine hesitancy during the early months after supply became available and its impact on the government’s overall rollout, however with so much of the focus on getting jabs in arms, are we ignoring another potentially life-threatening form of hesitancy: the reduction and delaying of medical appointments?
Back in May 2020, just a few months into the pandemic, the Australian General Practice Alliance warned of a ‘tsunami of health problems’ that could arise due to patients postponing screening, pathology and other check-ups. And now, with many months of COVID restrictions under our belts and a glimpse of freedom on the horizon, is the tsunami about to hit?
We polled a group of GPs on our healthcare professionals panel to get a deeper understanding of what those on the front line of community healthcare are experiencing. The findings show that while the nation focuses its attention on COVID, there are other acute health problems that could be going undetected.
Majority of GPs report reduction in appointments
When asked if they believed patients were less likely to book a medical appointment due to the COVID-19 situation, 69% of GPs agreed they believed this is occurring. This supports research carried out by the Continuity of Care Collaboration, which found that 1 in 3 respondents had delayed or avoided a visit to a GP in the previous three months.
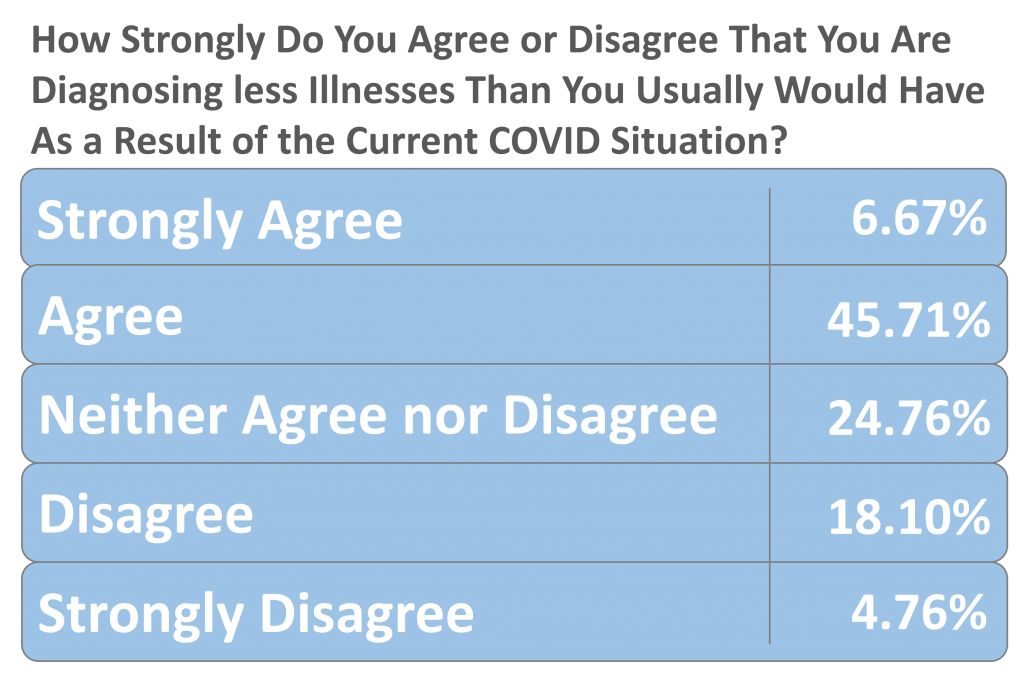
So does this mean diagnoses are being missed? Until appointment levels return to normal it may be hard to quantify the overall long-term impact of healthcare hesitancy. However, more than half of the GPs we polled (52%) said they were diagnosing fewer illnesses as a result of the pandemic
The impact of late diagnosis
Overall, 84% of practitioners believed COVID was deterring patients from accessing treatments for ailments or illnesses.
The knock-on effects of delayed diagnosis could potentially be felt for months and years to come. 63% of GPs said patients were presenting with symptoms and illnesses at a more advanced stage due to delaying appointments during the pandemic.
In recent months there have been increased calls for a greater focus on the illnesses and conditions that have been under-reported since the pandemic started, with some commentators calling for greater perspective when it comes to reporting the risks associated with COVID in comparison to other chronic diseases.
As of the end of last week, Australia sat in position 113 in the global table for COVID deaths, with 1,231 total deaths. All deaths from disease are devastating for families and loved ones, but by focusing so much attention on the urgent issue of COVID, are we neglecting other important health concerns?
In a recent podcast broadcast hosted by the University of Sydney, Associate Professor Melody Ding, of the university’s School of Public Health said:“ So the WHO estimates of death from COVID is more than three million. But at the same time, ischemic heart disease killed more than 13 million and stroke killed more than 9 million. So this is the context out there. And we must take the same initiative efforts and consolidate consulted efforts to address non-communicable disease continuously beyond COVID-19 pandemic.”
Mental health diagnoses increase, despite drop in appointments
While much of the focus of the press briefings and reporting on the pandemic has been on case numbers and death rates, there’s a rising concern among health professionals about the mental health emergency prompted by the restrictions and broader impacts of COVID.
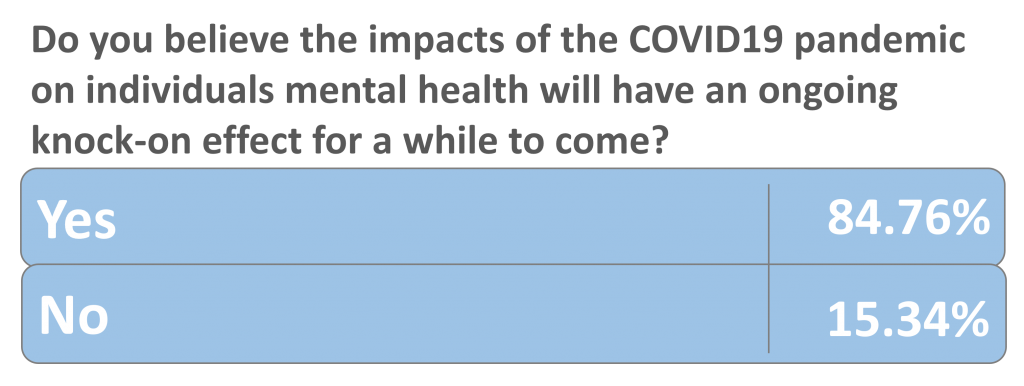
Although more than two thirds of the GPs we polled said patients were less likely to book appointments, they also reported seeing more patients presenting with mental health symptoms among those whom they did see.
Furthermore, 85% said they believed the pandemic would have an impact on mental health for some time to come.
So, what changes in symptoms are GPs now seeing?
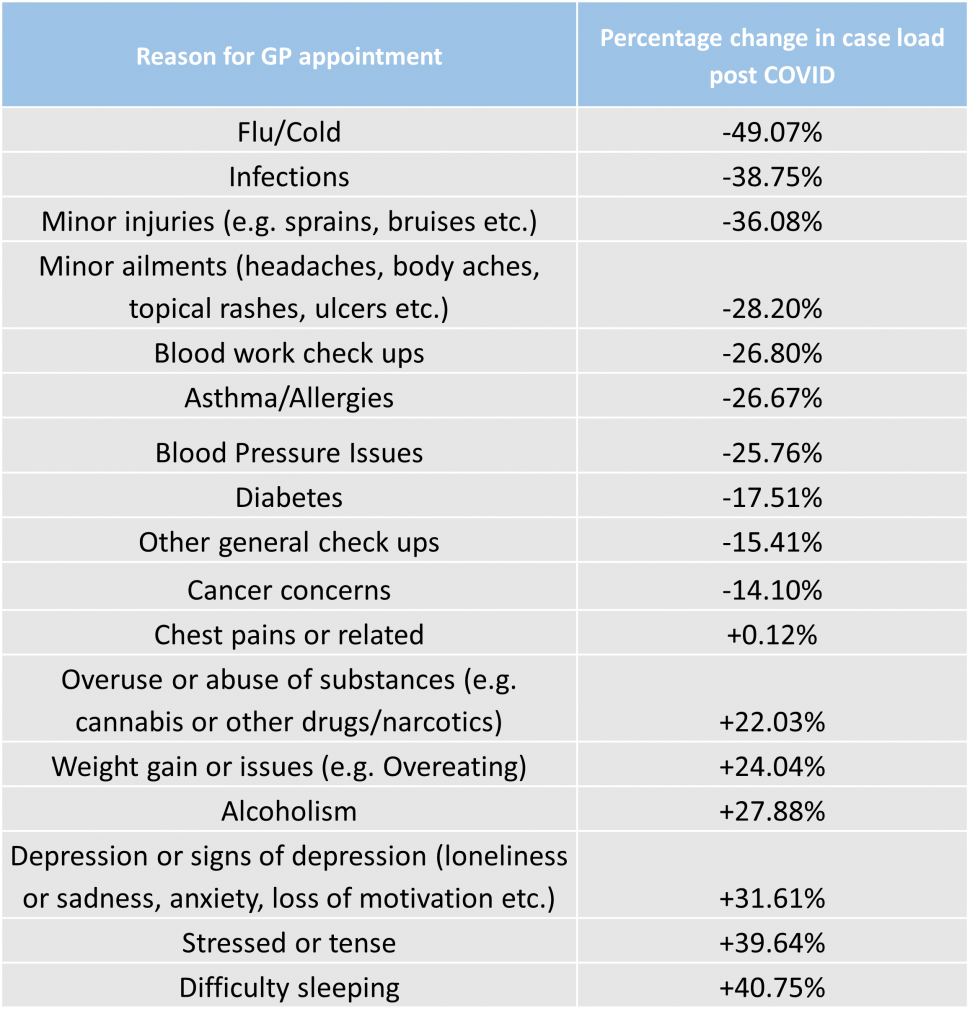
We asked the panel about the numbers of patients they had seen for specific conditions both pre and post COVID. Their responses show a shift in the types of symptoms people are now seeking consultations for.
There was a decrease in the number of patients the GPs reported seeing post COVID for minor ailments such as allergies, cold and flu and infections – as well as for more serious concerns such as diabetes or cancer. However, when asked about mental health conditions, there was an increase in the number of patients GPs reported seeing – with difficulty sleeping (+41%), stress (+40%) and signs of depression (+32%) showing the biggest increases.
‘It’s never been easier to access your GP’
One of the biggest concerns to arise among healthcare practitioners during the pandemic is hesitancy in accessing expert care and diagnostic services. While skipping the doctor’s office if you have cold or flu symptoms may not have any lasting effects on many patients, putting off visiting a GP for symptoms that could turn out to be cancer can have a significant impact on health outcomes.
And despite the introduction of telehealth at the start of the pandemic last year, which opens up appointments to anyone unable to attend in person, there are fears among practitioners that there isn’t a level playing field when it comes to accessing these services.
70% of the GPs we polled agreed some people who needed to book healthcare consultations were being left behind due to not being in a position to access digital services. This is often due to some patients not having the support or technology they need to book telehealth appointments, and in some cases a lack of awareness of the services available.
The issue of healthcare hesitancy in Australia has prompted a large-scale response from GP groups, including a major campaign from the Royal Australian College of General Practitioners to encourage patients to continue seeing GPs throughout the pandemic.
After the campaign launched, RACGP president Dr Harry Nespolon said: “General practice is the first port of call for people when it comes to their health…
It’s important that people realise that it’s never been easier to access your GP – online, by phone, or in person.”
KEY FINDINGS
69% of respondents agree patients are less likely to book an appointment as a result of the COVID-19 situation.
53% of practitioners believe they are diagnosing fewer illnesses due to the pandemic.
63% of those polled say patients are making appointments when their conditions are at a more advanced stage
92% of GPs believe there has been an increase in people exhibiting negative mental health symptoms since the pandemic began
Ekas spoke to 180 General Practitioners on its panel Medical Opinion Leaders in September 2021