A wide ranging survey of Australian GPs by EKAS market research shows that use of the MyHealthRecord (MHR) system is high, with four out of five doctors utilising the online summary in their practices. In total 83% of GPs have been won over by the initiative, which has been up and running since 2018 following initial trials in 2016.
With a prevailing climate of concern around digital data privacy, which saw around 2.5 million Australians opt out of the scheme, the high take up rate is a strong endorsement of the initiative from Australia’s medical practitioners.
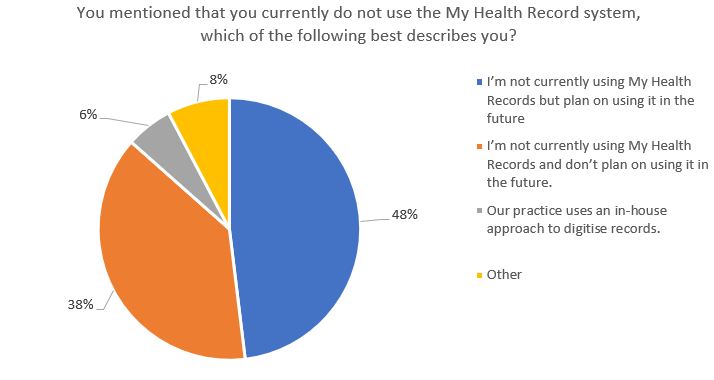
The number of GPs employing MHRs is also likely to swell with nearly half of those who said they do not currently use it stating they intend to employ it in the future. But that will leave around 7.5% of GPs not on the system – representing tens of thousands of patients Australia-wide.
What’s the take up rate and who should choose?
Following initial trials in 2016, from July 16 last year through to January 31 Australians were subject to an opt-out period where they could decline a MHR.
At the conclusion of this period, roughly 2.5 million Australians or about 10% of the population declined to have a MHR created, with the remainder automatically having a record created for them.
And while the government might have figured that an opt-out initiative was likely to see fewer people actively declining an MHR, GPs weren’t overwhelmingly convinced this was the right approach.
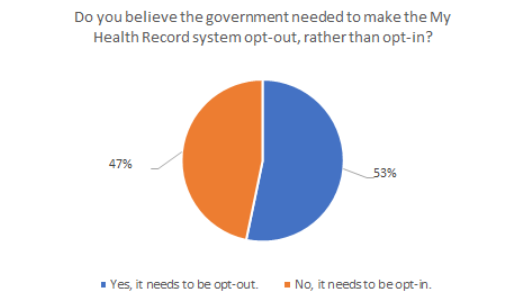
In fact, the question of how much autonomy individual Australians should be given over the creation of MHRs proved very divisive for the surveyed GP cohort. A roughly even split was recorded when GPs were asked whether the MHR should be opt-in (53%) as opposed to opt-out (47%), with a larger number ultimately feeling that records should not be created unless specifically asked for.
Curiously, GPs themselves seem considerably less inclined to commit details of their health to record than the general public. Just shy of half of those surveyed (48%) have personally opted out of the MHR with the remaining 52% happy to join the vast majority of their countrymen in creating an MHR.
Roughly 70% of those GPs who have opted out of an MHR said via an open-ended question that they either don’t have serious health issues or understand their own health well and don’t need to commit it to record.
Weighing up the pros and cons of the MHR
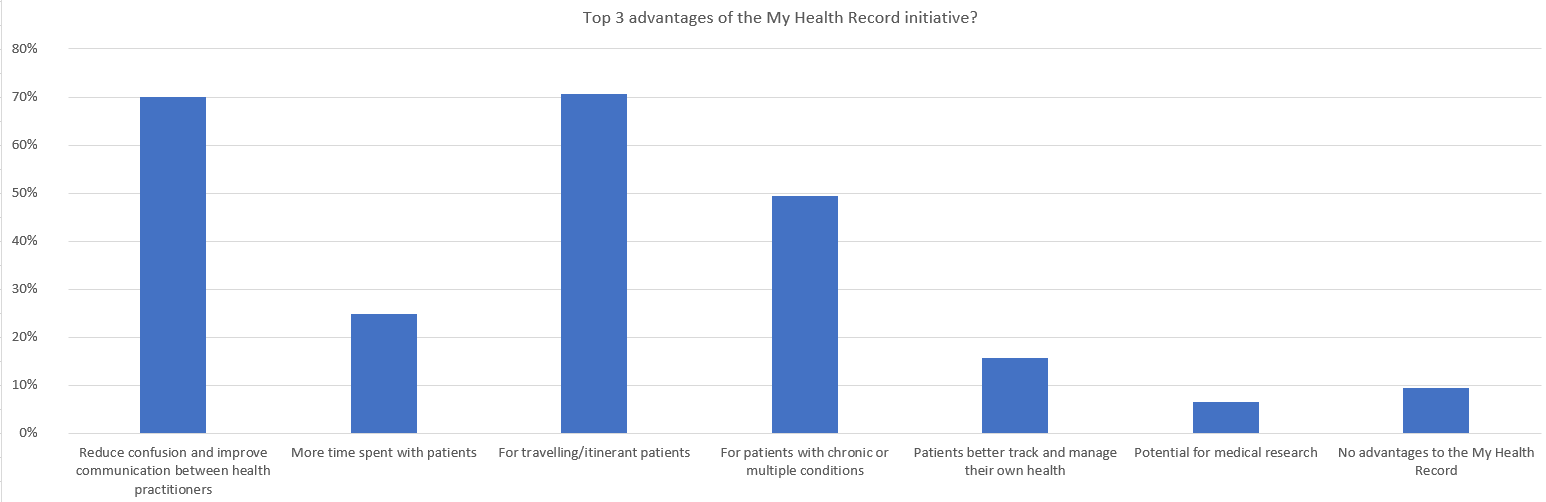
When the survey group was asked about the chief advantages of the MHR, two outcomes stood out as the perceived benefits. Some 71% of GPs could see the ‘benefit of using MyHealthRecord for travelling/itinerant patients who are expected to see several different healthcare providers, while 70% agreed that it had the ‘potential to reduce confusion and improve communication between health practitioners’. A further 49% said that it was beneficial ‘for patients with chronic or multiple medical conditions’.
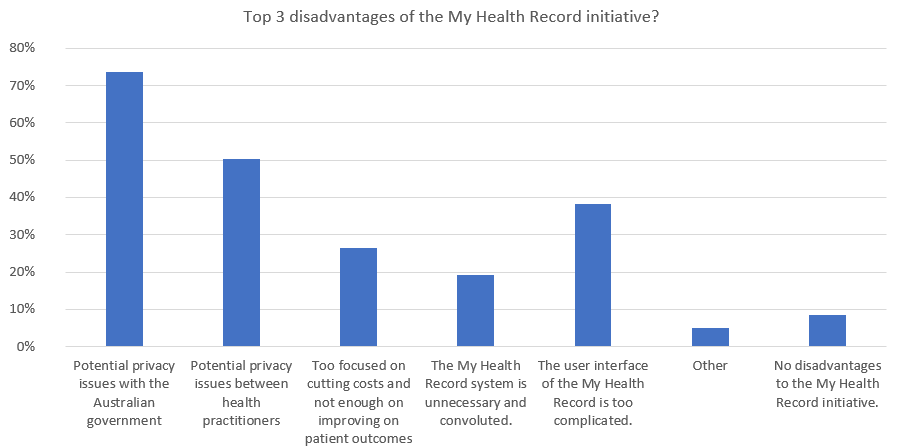
In terms of the drawbacks of the MHR, the results indicated the data-privacy conscious times we live in, with GPs strongly concerned about personal information finding its way into the wrong hands. Nearly three quarters (74%) of respondents cited ‘potential privacy issues with the Australian government’.
Interestingly, the next most concerning aspect for GPs – with a full 50% citing it – was ‘potential privacy issues between health practitioners’.
Privacy concerns aside, the next biggest drawback was more functional in nature with 38% stating ‘the user interface of the MHR is too complicated’.
Sharing second party data – better health outcomes or a recipe for disaster?
The question of using de-identified data for purposes outside record keeping drew a strong response from GPs, with some sources drawing moderate approval and others near universal condemnation.
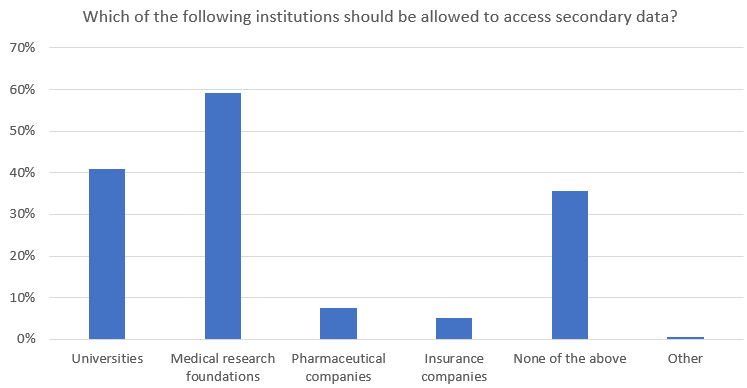
Perhaps unsurprisingly, GPs took a dim view of sharing data with pharmaceutical and insurance companies, even when de-identified. Just 8% of GPs were in favour of Big Pharma receiving such information, while 5% were happy with it in the hands of insurers.
The most approved source for willingly shared de-identified data was medical research foundations, but even these institutions only gained the backing of 59% of GPs. Another 41% of GPs were happy with data of this kind being shared with universities.
But there’s a strong school of thought amongst GPs that de-identified MHR information has no place being shared beyond the individual or doctor. Over a third of GPs (36%) opted for ‘none of the above’ when furnished with all sharing options in the survey.
Conclusions
Over 80% of Australian GPs have already welcomed patient MHRs into their practices and there are signs that this number may soon rise to over 90%, which is roughly in line with the number of Australians currently in possession of their own MHR.
High-profile data breaches which have dogged tech and other companies in recent years appear to have had an effect on GPs’ confidence in the ability to protect patient information. Roughly two in five of those surveyed are unhappy with the notion of de-identified MHR information being shared with any outside source.
Clearly, then, there is work to do for the government, technology providers and researchers to convince practitioners that they are capable of handling this most sensitive of data in order to help advance research and health outcomes.
The survey asked six questions (with two sub-questions) to Australia-based GPs who are part of EKAS market research’s medical panel. A total of 326 completed responses were received and constitute the sample for the results in this article. In terms of respondents, 59% identified as Metro GPs and 41% as regional, while 44.5% identified as male, 42.5% identified as female and 13% were unspecified.
