Diabetes has been cited as “the biggest challenge confronting Australia’s health system” as the number of those diagnosed with the disease continues to rise. But behind the stark headlines lies a desire among many patients to make conscious positive lifestyle changes and take control of their future health outcomes.
So what potential impact could these transformations have on the wellbeing of Australian diabetics and their families?
Diabetes today: a chronic disease rising steadily
There are an estimated 1.7 million Australians currently living with diabetes, 100,000 of whom have developed the condition in the past year.
According to Diabetes Australia, diabetes “is the fastest growing chronic condition in Australia; increasing at a faster rate than other chronic diseases such as heart disease and cancer”.
Although diabetes can be categorised into different types – Type 1, Type 2 and gestational diabetes – are three all increasing.
Managing diabetes: an emerging mindset
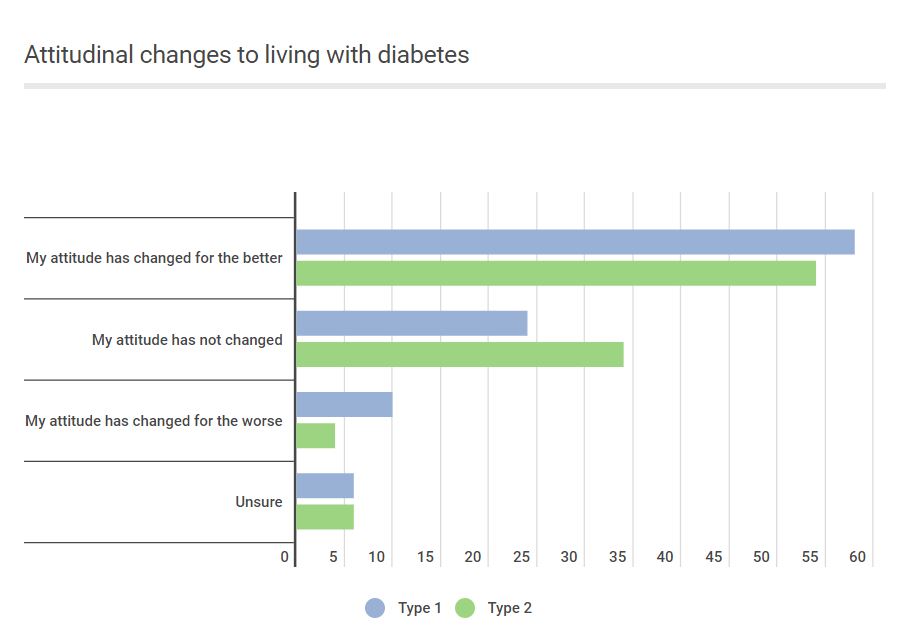
While the Australian stats are alarming, more than half of those living with diabetes say their attitudes have changed for the better in recent years. And not only this, more than two thirds say they can manage their condition “with ease”.
A recent Ekas poll of diabetes patients digs deeper into their attitudes towards living with the chronic disease and whether their feelings about treatment and prognosis have changed.
The most commonly felt emotion at diagnosis among diabetes patients was shock/surprise (21.9%), followed by feelings of devastation (12.4%), and concern/worry (11.8%). However, the experience of living with the condition and managing it on a day-to-day basis has led to a positive attitudinal shift among many of those polled.
55.71% of patients say their attitudes have changed for the better, while only 5.71% say their attitudes have changed for the worse.
The positive sentiment is further echoed in how patients feel about their future treatment. Almost two thirds (63.57%) of patients feel optimistic about the future and that their healthcare needs will be met; 25% feel confused or uncertain about whether their healthcare needs will be met; and 5% feel disheartened and do not believe their healthcare needs will be met in the future.
Though they both fall under the diabetes umbrella, type 1 and type 2 diabetes are significantly different diseases, with different risk factors and treatment plans. The survey also highlighted a slight disparity in attitude between the two groups.
Those with type 1 diabetes are generally less optimistic about their future needs and treatment; just over half (52.72%) saying they feel optimistic, compared to 66.67% of those with type 2 diabetes.
When it comes to managing their illness day to day, the picture for many patients is also a positive one. A majority (67.86%) of patients say they can manage their diabetes with varying degrees of ease. 31.43% report being able to manage the condition “with great ease”; 36.43% “with some ease”, and only 17.86% “with difficulty”. Again there is a small, and perhaps not unsurprising, disparity between the type 1 and type 2 patients. Type 1 patients are more likely to find managing the condition difficult (27.59%, compared to 15.31% of those with type 2).
The impact of diabetes on the lives of patients and their families
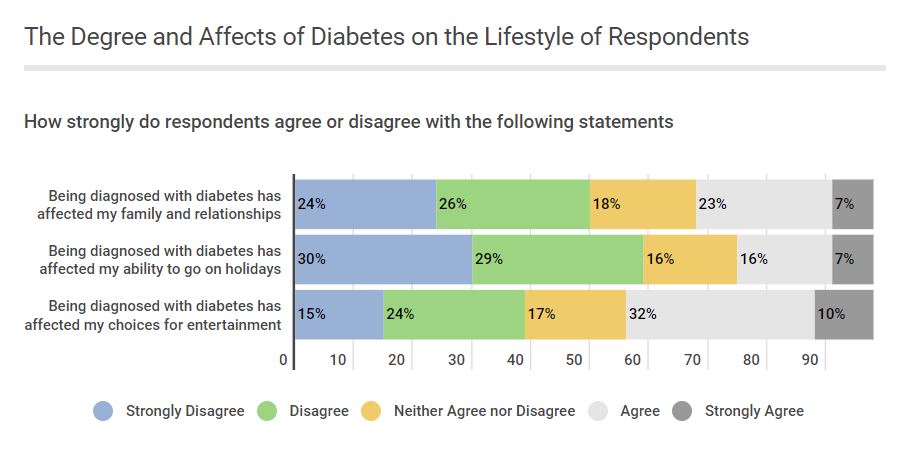
While many patients are facing the challenge of managing their diabetes with positivity, this doesn’t detract from the reality of living with a chronic disease. Life can become more restricted, and continually monitored – particularly when it comes to diet. And because diet and food is so closely linked to social life, it is no surprise that this was the area most affected by diabetes.
42.85% of patients agree their diagnosis has affected choices for entertainment and eating out, 30.71% say it has an impact on family and relationships, and 20.57% believe it affects their ability to go on holidays.
One respondent says they “don’t really enjoy going out anymore as it is too much hassle – everything is harder on holidays”.
Some of those polled also report experiencing some of the more severe side effects of diabetes, such as kidney problems and amputation.
The potential for complications and further chronic conditions as a result of diabetes cannot be ignored when dealing with a disease that affects such a large amount of the population. However, the ways in which patients are responding to their diagnoses could be cause for future optimism.
Early studies indicate that positive psychological states among patients can lead to better outcomes, which is further bolstered by the healthy lifestyle changes many diabetes patients adopt after diagnosis.
A new level of consciousness
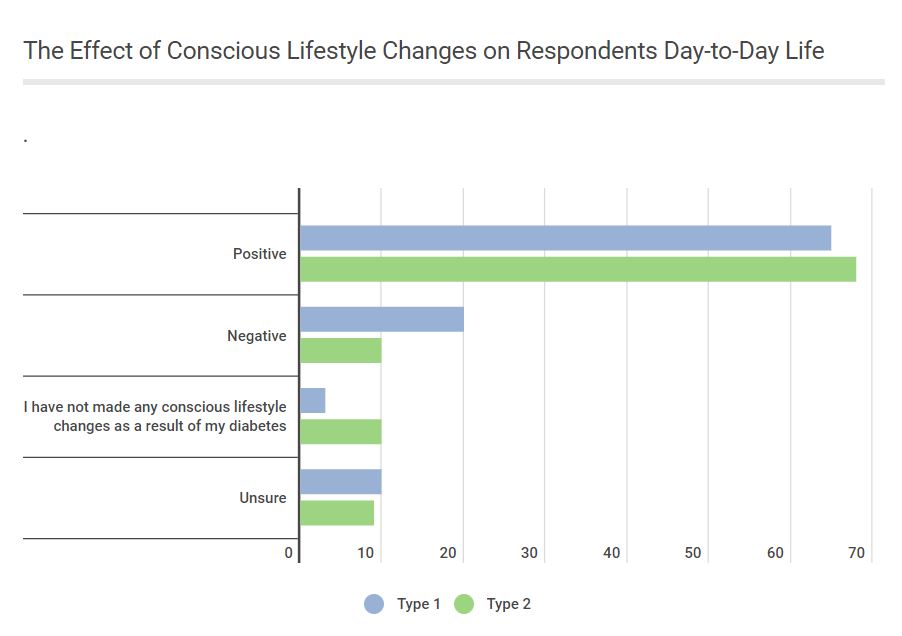
67.86% of the patients polled by Ekas report making positive, conscious lifestyle decisions as a result of being diagnosed with diabetes. The main focus of these decisions is around diet and eating habits.
Many also note that their diagnoses have improved the diet and exercise regimes of their entire families.
One respondent says they are now conducting “label research and analysis when shopping for groceries for the family” as well as modifying family meals and “ highlighting the effects of excessive sugar consumption to the children”.
This heightened mindfulness around diabetes, its triggers and the ways to manage it can not only have a positive knock-on effect for future generations of patients, but also on their families and loved ones.
One patient in the 40-45 age group comments: “I don’t like diabetes, but I have adapted to having diabetes and I do not and will not let it cause me to not live my life to the fullest I am able to.”
Ekas key findings:
Satisfaction levels with current treatment options are high among people with diabetes in Australia. 83.67% say they are either very satisfied or satisfied with their treatment. 13.61% feel neither satisfied or dissatisfied, 2.72% feel dissatisfied and no one polled feels very dissatisfied with their current treatment.
● Day-to-day management of diabetes is also under control for almost two thirds of patients. 31.43% of patients say they manage their diabetes “with great ease”; 36.43% “with some ease”, and 17.86% “with difficulty”. Type 1 patients are more likely to find managing the condition difficult (27.59%, compared to 15.31% of those with type 2).
● 63.57% of patients feel optimistic about their future and that their healthcare needs will be met; 25% feel confused or uncertain about whether their healthcare needs will be met; and 5% feel disheartened and do not believe their healthcare needs will be met in the future.
● 67.86% of patients have made positive conscious lifestyle changes since being diagnosed with diabetes. 12.86% of patients report making changes that have had a negative impact.
● 42.85% of patients agree their diagnosis has affected choices for entertainment and eating out, 30.71% say it has an impact on family and relationships, and 20.57% say it affects their ability to go on holidays.
● 55.71% of patients say their attitudes have changed for the better, while only 5.71% say their attitudes have changed for the worse.
● When it comes to how patients feel about their diabetes, 55.71% say their attitudes have changed for the better, 32.14% say their attitudes remain unchanged, 5.71% say their attitudes have changed for the worse.
The Ekas diabetes survey ran on Apple A Day Research polled 162 diabetes patients, 78% of whom reported being diagnosed with type 2 diabetes and 22% of whom reported being diagnosed with type 1 diabetes
